Milk Thistle Promotes Liver Detoxification
 The liver is a primary defense against daily toxins.
The liver is a primary defense against daily toxins.
People used to think that the main threat to their liver was alcohol.
Today's nemesis is obesity. The result is an epidemic crisis of non-alcoholic fatty liver disease (NAFLD).1
Liver-related deaths jumped 65% between 1999 and 2016.2,3
Milk thistle extract has demonstrated benefits for non-alcoholic fatty liver disease, alcoholic liver disease, and cirrhosis.4-7
When standardized extracts of milk thistle are combined with a phospholipid delivery system, absorption is significantly enhanced.
 What you need to know
What you need to know
- The liver is one of the largest organs in the body and is critical for numerous functions, including removing environmental and dietary toxins from the body.
- Liver disease is on the rise, affecting a large percentage of the population.
- Extracts of milk thistle contain a powerful blend of liver-protecting compounds that help defend against toxins and oxidative stress.
- Studies have demonstrated the ability of milk thistle extracts to protect the liver from a variety of causes of injury.
- Standardized extracts of milk thistle complexed to phospholipids provide the greatest absorption into body tissues.
 The public tends to assume that liver disease affects only those who have abused alcohol.
The public tends to assume that liver disease affects only those who have abused alcohol.
What few people know is that as many as 30% of all adults suffer from non-alcoholic fatty liver disease, mostly caused by obesity.
There has been an almost two-fold increase in non-alcoholic fatty liver disease since 1991. 1
Those whose diets consist of junk food and drinking sodas are falling victim to non-alcoholic fatty liver disease at alarming rates.8
The liver is one of the largest and most important organs in the body. It is susceptible to many sources of damage. These can include fatty liver disease infections, metabolic insults, and toxic poisonings including alcohol abuse.
Milk thistle extract has been shown to guard the liver from damage and reduce liver-related mortality.4,9-11
Factors behind Liver Disease
Poor diets, obesity, and other factors can lead to permanent liver damage. Chronic liver injury increases the risk for liver cancer, cirrhosis, and liver failure.
Here are some underlying correctable risk factors of the surging liver disease epidemic:
- Excess alcohol ingestion (especially without accompanying it with antioxidants like n-acetyl-cysteine).12-14
- Excess use of acetaminophen pain-relieving drugs (sometimes sold as Tylenol®).15-17
- Abdominal obesity and excess body weight that contributes to nonalcoholic fatty liver disease.18 Almost 40% of adults are clinically obese according to the Center for Disease Control and Prevention (CDC).1
Considering the critical role of the liver in human health, and the growing incidence of liver disease, researchers have focused on the capacity of milk thistle extract to inhibit the most common causes and pathologies of liver damage.
The Potent Liver-Protection Effects of Milk Thistle Extract
Extracts of milk thistle contain several natural compounds that demonstrate the ability to defend the liver from injury. These compounds offer multiple mechanisms of liver protection, including strong oxidant protection and anti-inflammatory properties.19,20
Here are some brief descriptions of studies looking at how milk thistle extract defends against some of the main drivers of liver disease.
Phospholipids: Improving the Bioavailability of Milk Thistle Extract
 Novel formulations of milk thistle extract have been developed that greatly improve the ability of the digestive system to absorb its beneficial compounds.
Novel formulations of milk thistle extract have been developed that greatly improve the ability of the digestive system to absorb its beneficial compounds.
By joining these compounds with natural phospholipids, such as phosphatidylcholine, the bioavailability of standardized extracts of milk thistle is greatly increased.37
This new delivery system has been shown both to increase entry of milk thistle's essential liver-protective compounds into the body and to maximize its beneficial effects.37
Non-Alcoholic Fatty Liver Disease
 Non-alcoholic fatty liver disease is characterized by the deposition of fatty compounds in the liver. As the name implies, it is not caused by alcohol abuse and can occur even in individuals with little or no alcohol intake.
Non-alcoholic fatty liver disease is characterized by the deposition of fatty compounds in the liver. As the name implies, it is not caused by alcohol abuse and can occur even in individuals with little or no alcohol intake.
The prevalence of this disease is increasing, closely following the increases seen in related disorders, such as diabetes, metabolic syndrome, and obesity.1 In fact, non-alcoholic fatty liver disease can occur in up to 90% of obese individuals. 21 Fatty liver disease is on track to soon surpass alcoholism and viral hepatitis as the most common cause of chronic liver disease.
Early in its course, fatty liver disease may go unnoticed. However, it can progress over time to cause significant fibrosis of the liver and ultimately result in liver cancer, cirrhosis, and/or liver failure.
Scientists have demonstrated that, in preclinical models, extracts of milk thistle are capable of changing the abnormal metabolism associated with non-alcoholic fatty liver disease, reducing the accumulation of fatty substances and protecting cells from oxidative damage and death. 22-24
The mechanism of this protection may involve altering gene expression related to lipid metabolism, mitochondrial function, and antioxidant mechanisms.
In multiple studies of humans with fatty liver disease, intake of milk thistle extract has been associated with a reduction in fat deposition and improved enzyme blood markers of liver damage. 25-27
A meta-analysis of eight trials concluded that milk thistle extract effectively lowered liver enzymes, compared to controls, in non-alcoholic fatty liver disease patients.28
In randomized controlled trials, non-alcoholic fatty liver disease subjects treated with milk thistle extract for 48 weeks had markedly less fibrosis than those who received placebo.25,26,29
Alcohol and Other Liver Toxins
 The liver is susceptible to an array of dangerous toxins known as hepatotoxins, including Amanita mushrooms, acetaminophen, arsenic, alcohol, and others.5,30,31
The liver is susceptible to an array of dangerous toxins known as hepatotoxins, including Amanita mushrooms, acetaminophen, arsenic, alcohol, and others.5,30,31
Research shows that milk thistle extract prevents liver damage when given before or during the exposure to a liver toxin.9,10,32,33
andlt;pstyle="text-align: justify;"andgt;A common toxic cause of liver injury is alcohol abuse, and it appears to be on the rise, particularly in young adults.2,3 The best prevention of alcoholic liver disease is cessation of alcohol intake, but clinical trials have shown that milk thistle extract can even benefit people who've already developed the condition.6,11
One of these trials evaluated three different dose levels and found that the highest doses, 360 mg per day of the milk thistle extract preparation, resulted in the greatest improvement in liver enzyme levels.6 Another study showed that a group of patients with alcohol-induced liver disease who were treated with milk thistle extract showed improvements in liver enzymes and liver pathology.7
New studies show even what some people consider moderate alcohol ingestion can inflict an injurious impact.34 One might consider supplementing with milk thistle extract, n-acetyl-cysteine, vitamins B1, and C before ingesting ethanol.35
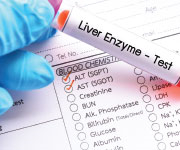
Liver Enzymes as Markers of Liver Injury
 Measurement of liver enzyme levels is an important tool that clinicians and researchers use to identify ongoing liver injury.
Measurement of liver enzyme levels is an important tool that clinicians and researchers use to identify ongoing liver injury.
These proteins, including AST and ALT, are normally present inside liver cells. However, when any pathology causes damage to liver cells, the levels of these enzymes rises in the blood, detectable on a simple blood test.
Elevated liver enzyme levels are therefore a useful marker of liver disease and can help to track response to treatment.
Milk thistle extracts have been found to decrease liver enzyme levels in many clinical studies, indicating protection from various types of liver injury.6,28,38-41
Cirrhosis
Cirrhosis is the end-stage of chronic liver injury. It can occur following years of ongoing liver injury from a number of possible causes, including viral and alcoholic hepatitis.

Cirrhosis is generally considered irreversible. But scientists have observed promising improvements with milk thistle extract in clinical trials.
In one such trial of 60 patients with alcoholic liver cirrhosis, those randomized to receive 450 mg of a milk thistle extract daily benefited from a reduction in a marker of liver fibrosis, along with improvements in oxidant reduction.36
Also, in a study of alcoholic and non-alcoholic patients with cirrhosis, 420 mg of milk thistle extract per day was associated with a higher overall four-year survival. This study showed that 58% of subjects supplementing with milk thistle survived compared to only 39% survival in controls (who did not receive milk thistle extract).4 The greatest clinical improvement was observed in alcoholics.
Summary
Among its myriad functions, the liver is crucial for detoxification, purifying the body of various toxic substances. As it performs these functions, the liver is itself prone to injury.
Acting through multiple mechanisms, compounds in milk thistle extract have the ability to protect the liver against toxins and metabolic disorders.
Health-conscious individuals can boost their body's absorption of these protective compounds by taking standardized extracts of milk thistle that have been made more bioavailable via a phospholipid delivery system.
Material used with permission of Life Extension. All rights reserved.
- Le MH, Devaki P, Ha NB, et al. Prevalence of non-alcoholic fatty liver disease and risk factors for advanced fibrosis and mortality in the United States. PLoS One. 2017;12(3):e0173499.
-
Bakalar N. More Americans are dying of cirrhosis and liver cancer. New York Times. July 23, 2018: D4.
-
Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817.
-
Ferenci P, Dragosics B, Dittrich H, et al. Randomized controlled trial of silymarin treatment in patients with cirrhosis of the liver. J Hepatol. 1989 Jul;9(1):105-13.
-
Federico A, Dallio M, Loguercio C. Silymarin/Silybin and Chronic Liver Disease: A Marriage of Many Years. Molecules. 2017 Jan 24;22(2).
-
Vailati A, Aristia L, Sozze E, et al. Randomized open study of the dose-effect relationship of a short course of IdB 1016 in patients with viral or alcoholic hepatitis. Fitoterapia. 1993;64(3):219-28.
-
Salmi HA, Sarna S. Effect of silymarin on chemical, functional, and morphological alterations of the liver. A double-blind controlled study. Scand J Gastroenterol. 1982 Jun;17(4):517-21.
-
Yasutake K, Kohjima M, Kotoh K, et al. Dietary habits and behaviors associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2014 Feb 21;20(7):1756-67.
-
Enjalbert F, Rapior S, Nouguier-Soule J, et al. Treatment of amatoxin poisoning: 20-year retrospective analysis. J Toxicol Clin Toxicol. 2002;40(6):715-57.
-
Mengs U, Pohl RT, Mitchell T. Legalon(R) SIL: the antidote of choice in patients with acute hepatotoxicity from amatoxin poisoning. Curr Pharm Biotechnol. 2012 Aug;13(10):1964-70.
-
Saller R, Brignoli R, Melzer J, et al. An updated systematic review with meta-analysis for the clinical evidence of silymarin. Forsch Komplementmed. 2008 Feb;15(1):9-20.
-
Torok NJ. Update on Alcoholic Hepatitis. Biomolecules. 2015 Nov 2;5(4):2978-86.
-
Ozaras R, Tahan V, Aydin S, et al. N-acetylcysteine attenuates alcohol-induced oxidative stress in the rat. World J Gastroenterol. 2003 Jan;9(1):125-8.
-
Khoshbaten M, Aliasgarzadeh A, Masnadi K, et al. N-acetylcysteine improves liver function in patients with non-alcoholic Fatty liver disease. Hepat Mon. 2010 Winter;10(1):12-6.
-
Watkins PB, Kaplowitz N, Slattery JT, et al. Aminotransferase elevations in healthy adults receiving 4 grams of acetaminophen daily: a randomized controlled trial. JAMA. 2006 Jul 5;296(1):87-93.
-
van Mil AH, Janssens AR. [Acetaminophen use by chronic alcohol abusers: a therapeutic dose may be too much for the liver]. Ned Tijdschr Geneeskd. 2001 Sep 29;145(39):1873-6.
-
Available at: https://library.lsuhscs.edu/am_rpt/media/files/10232009.pdf. Accessed October 9, 2018.
-
Available at: https://www.niddk.nih.gov/about-niddk/research-areas/liver-disease. Accessed October 15, 2018.
-
Polyak SJ, Morishima C, Lohmann V, et al. Identification of hepatoprotective flavonolignans from silymarin. Proc Natl Acad Sci U S A. 2010 Mar 30;107(13):5995-9.
-
Saliou C, Valacchi G, Rimbach G. Assessing bioflavonoids as regulators of NF-kappa B activity and inflammatory gene expression in mammalian cells. Methods Enzymol. 2001;335:380-7.
-
Brunt EM, Wong VW, Nobili V, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers. 2015 Dec 17;1:15080.
-
Ni X, Wang H. Silymarin attenuated hepatic steatosis through regulation of lipid metabolism and oxidative stress in a mouse model of nonalcoholic fatty liver disease (NAFLD). Am J Transl Res. 2016;8(2):1073-81.
-
Vecchione G, Grasselli E, Cioffi F, et al. The Nutraceutic Silybin Counteracts Excess Lipid Accumulation and Ongoing Oxidative Stress in an In Vitro Model of Non-Alcoholic Fatty Liver Disease Progression. Front Nutr. 2017;4:42.
-
Guo Y, Wang S, Wang Y, et al. Silymarin improved diet-induced liver damage and insulin resistance by decreasing inflammation in mice. Pharm Biol. 2016 Dec;54(12):2995-3000.
-
Federico A, Trappoliere M, Tuccillo C, et al. A new silybin-vitamin E-phospholipid complex improves insulin resistance and liver damage in patients with non-alcoholic fatty liver disease: preliminary observations. Gut. 2006 Jun;55(6):901-2.
-
Loguercio C, Andreone P, Brisc C, et al. Silybin combined with phosphatidylcholine and vitamin E in patients with nonalcoholic fatty liver disease: a randomized controlled trial. Free Radic Biol Med. 2012 May 1;52(9):1658-65.
-
Cacciapuoti F, Scognamiglio A, Palumbo R, et al. Silymarin in
non alcoholic fatty liver disease. World J Hepatol. 2013 Mar 27;5(3):109-13. -
Zhong S, Fan Y, Yan Q, et al. The therapeutic effect of silymarin in the treatment of nonalcoholic fatty disease: A meta-analysis (PRISMA) of randomized control trials. Medicine (Baltimore). 2017 Dec;96(49):e9061.
-
Wah Kheong C, Nik Mustapha NR, Mahadeva S. A Randomized Trial of Silymarin for the Treatment of Nonalcoholic Steatohepatitis. Clin Gastroenterol Hepatol. 2017 Dec;15(12):1940-9 e8.
-
Hackett ES, Twedt DC, Gustafson DL. Milk thistle and its derivative compounds: a review of opportunities for treatment of liver disease. J Vet Intern Med. 2013 Jan-Feb;27(1):10-6.
-
Surai PF. Silymarin as a Natural Antioxidant: An Overview of the Current Evidence and Perspectives. Antioxidants (Basel). 2015 Mar 20;4(1):204-47.
-
Clichici S, Olteanu D, Filip A, et al. Beneficial Effects of Silymarin After the Discontinuation of CCl4-Induced Liver Fibrosis. J Med Food. 2016 Aug;19(8):789-97.
-
Clichici S, Olteanu D, Nagy AL, et al. Silymarin inhibits the progression of fibrosis in the early stages of liver injury in CCl(4)-treated rats. J Med Food. 2015 Mar;18(3):290-8.
-
Available at: https://www.cancer.gov/about-cancer/causes-prevention/risk/alcohol/alcohol-fact-sheet. Accessed, October 16.
-
Available at: https://www.lifeextension.com/Magazine/2011/12/Link-Between-Alcohol-and-Cancer-Death/Page-01. Accessed October 16, 2018.
-
Lucena MI, Andrade RJ, de la Cruz JP, et al. Effects of silymarin MZ-80 on oxidative stress in patients with alcoholic cirrhosis. Results of a randomized, double-blind, placebo-controlled clinical study. Int J Clin Pharmacol Ther. 2002 Jan;40(1):2-8.
-
Polachi N, Bai G, Li T, et al. Modulatory effects of silibinin in various cell signaling pathways against liver disorders and cancer - A comprehensive review. Eur J Med Chem. 2016 Nov 10;123:
577-95. -
Buzzelli G, Moscarella S, Giusti A, et al. A pilot study on the liver protective effect of silybin-phosphatidylcholine complex (IdB1016) in chronic active hepatitis. Int J Clin Pharmacol Ther Toxicol. 1993 Sep;31(9):456-60.
-
Loguercio C, Festi D. Silybin and the liver: from basic research
to clinical practice. World J Gastroenterol. 2011 May 14;17(18):
2288-301. -
Marcelli R, Bizzoni P, Conte D, et al. Randomized controlled study of the efficacy and tolerability of a short course of IdB 1016 in the treatment of chronic persistent hepatitis. Eur Bull Drug Res. 1992;1:131-5.
-
Moscarella S, Giusti A, Marra F, et al. Therapeutic and antilipoperoxidant effects of silybin-phosphatidylcholine complex in chronic liver disease: preliminary results. Curr Ther Res. 1993;53:98-102.